Withdrawal of Warmth: Controversial or Therapeutic?
A brief response from a DBT therapist about the DBT strategy of “withdrawal of warmth.”
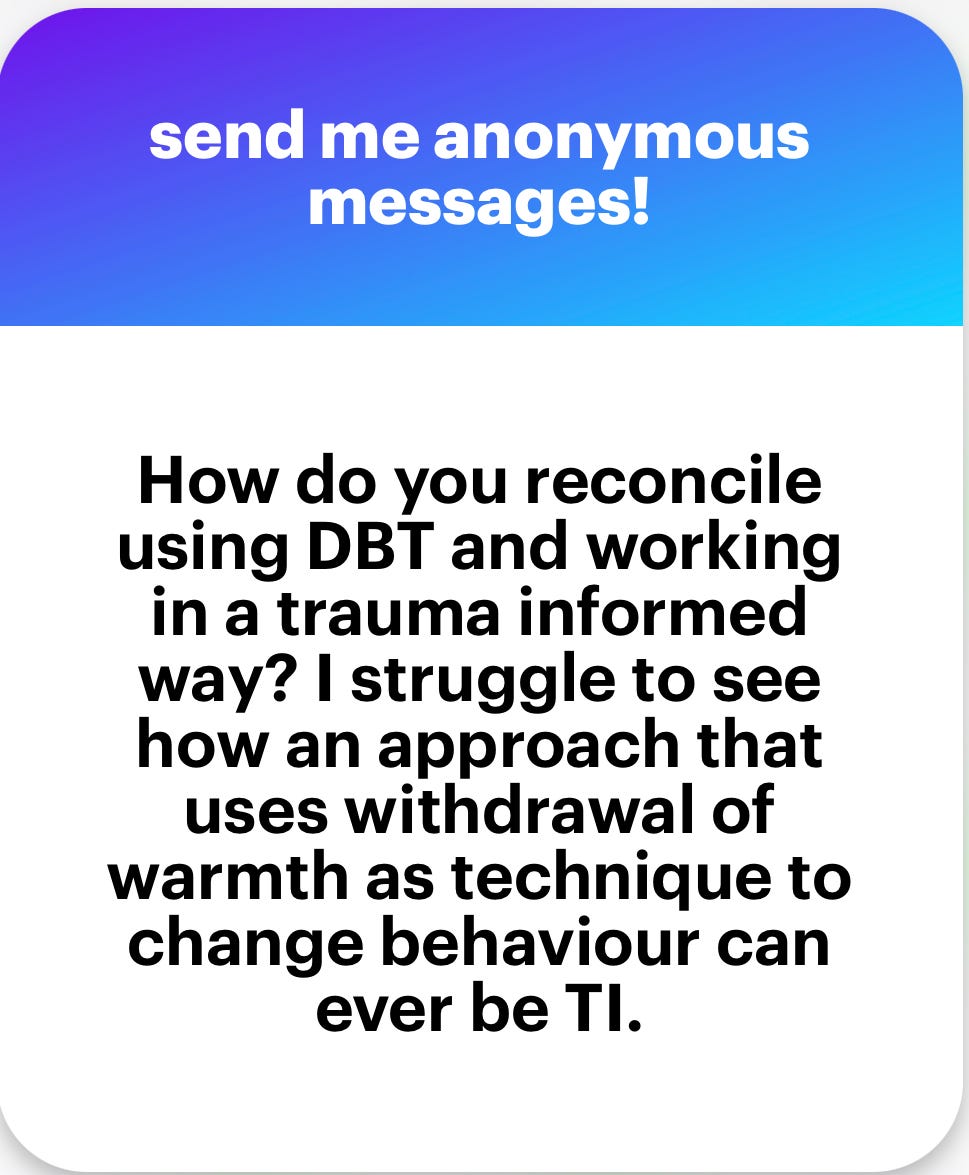
This blog piece came about after I was asked the following question in one of my anonymous Q&A sessions on my Instagram account:
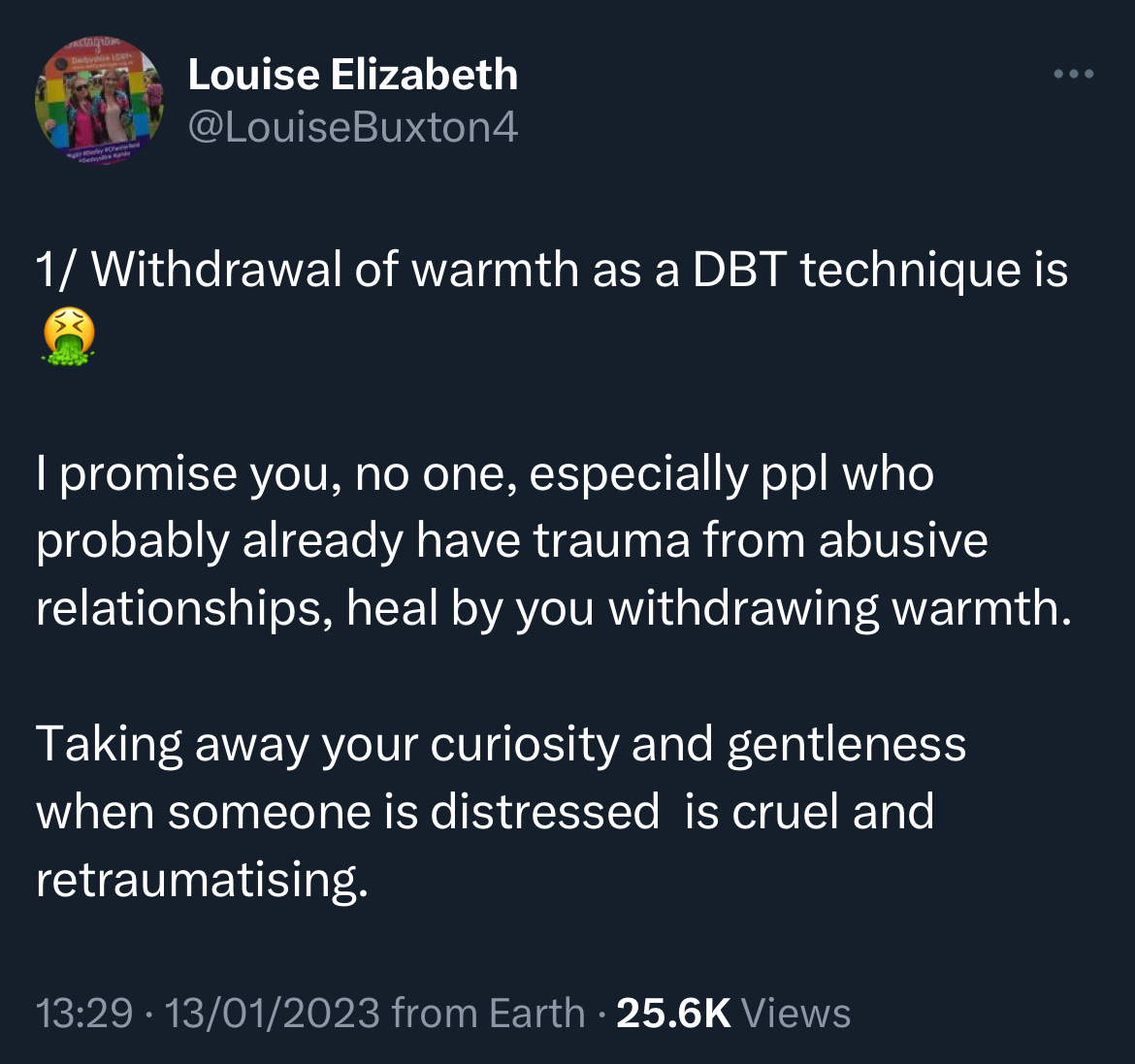
This is not the first time I have seen the subject of “withdrawal of warmth” raised on social media. A few months ago, it appeared to be the subject of discussion on several Twitter threads (see an example below - if you type “Twitter” and “withdrawal of warmth” into Google you get Twitter threats, blogs, and Reddit forms about this).
At the time I thought about responding but given the fact that Twitter can be a hotbed of reactivity and that the topic is one of contention that sparked a strong response in some, I held off. However, having been asked about it directly it now feels more appropriate to give a practitioner’s view of the DBT technique of “withdrawal of warmth”. I must admit, given the nature of the responses like the one above I have been a bit apprehensive about writing this. However, I think it is important to offer another perspective.
And it is worth emphasising that this is just that: a practitioner’s view. The word “dialectical” (the “D” in DBT) means “a discourse between two or more people holding different points of view about a subject but wishing to establish the truth through reasoned argumentation”. Basically, a) people can hold different and opposing views; b) there is truth and validity in both of those views; c) those views can and do exist at the same time, and d) it might be possible to find a middle ground. Therefore, with this blog, it is not my intention to argue that the views of those who disapprove of or question the use of “withdrawal of warmth” are incorrect or invalid. Indeed, as a DBT practitioner it is important to acknowledge that those views have their validity; their truth as it were. My aim here is to give context and present the other view of why and how the therapist strategy of “withdrawing of warmth” is used.
As a start, though, it might be worth giving a very potted overview of what DBT is.
What is DBT?
DBT (or more formally, Dialectical Behaviour Therapy) is a model of therapy designed specifically to help individuals with borderline personality disorder (BPD) who engage in self-harm and/or suicidal behaviour. DBT was developed by Marsha Linehan in the 1970s. Linehan, who herself has been diagnosed with BPD, emphasises how trauma or an “invalidating environment” contributes to the development of BPD. Thus, DBT was designed to work with individuals who have experienced significant trauma. It is a form of cognitive behaviour therapy that focuses more on developing behavioural skills to help DBT clients become aware of their triggers, thoughts and emotions, and manage their urges and harmful actions.
As noted above, DBT is all about trying to think of opposing positions (sometimes referred to as “poles”) of a situation while then trying to find a middle ground (or synthesis) between those two poles. Two poles that DBT clients often occupy at once are feeling that they can do nothing about their situations while also having difficulty accepting things as they are or of what happened in the past. Therefore, DBT focuses on teaching skills of change (to have more control over their current difficulties and life) and acceptance (of things that cannot be changed, which if held onto may keep them tethered to hurtful experiences of the past). The skills taught in DBT fall into four main modules: mindfulness (i.e., improved ability to focus on the here and now without judgement), emotional regulation (i.e., improved ability to recognise emotional responses and ways in which to manage those), distress tolerance (i.e., managing overwhelming crises in a way that reduces harm and/or unhelpful outcomes), and interpersonal effectiveness (i.e., improved communication skills).
As part of the therapy, a DBT client is expected to attend both a skills group session and an individual therapy session per week. The skills group focuses on teaching new skills, while individual therapy focuses on treatment goals, with priority given to reducing self-harm and suicidal behaviours, then targeting therapy-interfering behaviours (as these can get in the way of therapy and therefore increase a DBT client’s risk to themselves), and quality-of-life interfering behaviours.
Assumptions about Clients
DBT operates on several assumptions about clients that exist on opposing dialectical poles. It assumes that DBT clients harm themselves because they are “living in hell” due to the difficulties they face; however, they also want to pursue a “life worth living,” which is why they seek therapy. Another assumption is that while DBT clients are trying their best, they must also try harder. And a final assumption is that while DBT clients did not cause their difficulties, it is their responsibility to address them. It is the role of the therapist then to help clients move from one pole to the other. For example, to help them move “out of hell” and closer to goals they have for their “life worth living”; to acknowledge that they are doing their best, but pushing them to do more, try harder, learn new skills; and to help them take accountability for the choices they make in relation to their well-being.
DBT clients can struggle with learning and practising new skills due to challenges with emotional regulation, concerns about the difficulty of acquiring new skills, and a certain level of comfort in relying on old behaviours despite their potentially lethal consequences (all of which are completely understandable and expected). However, if clients do not actively learn or practice their new skills, they will not experience the intended benefits of therapy. These struggles are known as therapy-interfering behaviours (e.g., refusal to practice new skills, maintain skills diaries, repeated lateness and/or absence from group and/or individual sessions, significant disruption to group and/or individual session, persistent statements to end one’s life, an apathetic or cavalier approach to ending self-injurious behaviour, etc.), which can become the focus of an individual therapy session if necessary. Therapy-interfering behaviours are examined in-depth to understand their underlying reasons and find ways to reduce them, thereby enabling DBT clients to access the benefits of therapy. If clients refuse to engage in addressing therapy-interfering behaviours or continue to display them despite attempts to understand and reduce them, therapists can use a strategy known as the withdrawal of warmth to further deal with the issue.
Withdrawal of Warmth
Contrary to the beliefs expressed on social media, withdrawal of warmth in DBT does not (as far as I am aware and in all the time I have ever known about it) involve therapists being cruel or replicating past abusive behaviours. This is not to say that individual therapists may behave in this way (anything is possible and even therapists can intentionally cause harm). But at its core, DBT prioritises empathy and validation of a client’s lived experience while acknowledging the difficulties they face (there are seven levels of validation taught in DBT – seven – that’s how much DBT values validation). However, therapists also need to be aware that consistent therapy-interfering behaviours hinder progress and may impede clients’ well-being.
Withdrawal of warmth is a strategy to break this cycle, and it simply means therapists may need to adopt a more serious, solemn, grave, matter-of-fact, or irreverent stance, rather than a warm and encouraging one. This could involve openly and honestly expressing their frustration about being stuck (known as “radical genuineness,” which can also be used during moments of a client’s improvement), or highlighting concerns about the potentially fatal consequences if clients do not change their harmful behaviours (known as “plunging where angels fear to tread”). The use of irreverence is used on the basis that while DBT clients have elements of fragility about them they are also more robust than they might think, especially given that they are still trying the best they can and surviving while “living in hell”.
I guess the idea is that when trying to help someone who engages in harmful and life-threatening behaviours, empathy and validation are only one part of the solution. Guidance, boundaries and highlighting the seriousness of potential consequences are the other part. As an example (and please don’t think I am trying to infantilise adults, I am not – it is just a similar principle to help illustrate a point), when we think of teaching children about the world, if they are engaging in dangerous behaviour we don’t simply take an empathic and validating stance. When a child is heading towards a plug point with a metal fork we intervene. Initially, we may be able to empathise and validate the child’s need to explore the world and try out new things, but we also aim to highlight the dangers of what they have tried to do. However, if the child continues trying to stick the fork in the plug despite our empathic explanation, we may have to become more severe, serious, or stern, use a different tone, or remove the child from the dangerous area. This could also be viewed as the withdrawal of warmth because we are no longer communicating with the child in the same warm and empathic way we were. Yet the change in tone and using a different strategy becomes necessary to ensure the child is safe. This comes from a place of caring and love for the child, not because we want to be punitive or harsh.
Similarly, if a DBT client continues to engage in life-threatening behaviour a DBT therapist may need to change tact in order to get the point across. And as with the example above, this change of tact and the seriousness with which it is delivered does not come from a place of wanting to harm or hurt the client but from a place of caring and wanting the client to improve (and in the more extreme cases, stay alive). It is absolutely possible that DBT clients can perceive this change of tact as overwhelming or as criticism; at the same time, DBT therapists would rather have a rupture to the relationship which can be repaired than have a client hurt themselves significantly or fatally. With this in mind, guidance on the use of withdrawal of warmth emphasises that it is only used if extremely necessary; its use is dependent on the nature of the therapeutic relationship between client and therapist; and should only be used briefly and immediately followed by continued warmth and concern.
So, how do I reconcile practising DBT, a form of therapy that uses the withdrawal of warmth? Well, I guess I understand its use and the reason behind it. I know it is only used when clients and therapists are stuck; when warmth and validation may have reached their limit at a specific moment in the therapeutic journey and something needs to shift. I know it is used only when necessary and that it comes from a place of genuine care and concern. I know I would only ever use it if I knew I had a strong enough rapport with a client. And I know that I would rather be serious, grave, irreverent, or call a spade a spade for a moment than have a client do further harm to themselves.
Like most things, I think I have rambled on for quite a while now, potentially ad nauseam, so I will stop there. Hopefully, this has given some context and rationale for the use of withdrawing warmth in DBT therapy. Again, this blog was written to offer the other side of the pole, but the decision about whether you think withdrawing warmth is controversial or therapeutic is down to you. I am only one therapist with a view, and it is not to say that other DBT therapists share my views, or indeed that you, good reader, will or should.
As always, I would love to hear your thoughts on this. If there is anything you would like to clear up or challenge me on, please feel free to get in touch. You can either leave a comment here or come find me on my Instagram account.
Take care,
Nice-ish.




Thank you for this article. I found it really interesting. I think I understand the concept but wonder if you could provide a real-life example of when you have used this strategy? 🙏🏼
Nope. This is abusive.